Mindfulness reduces self-blame
Mindfulness-based cognitive therapy reduces activation in brain regions related to self-blame in patients in remission from depression
New research suggests mindfulness-based cognitive therapy protects remitted depressed patients from relapse by reducing tendencies toward self-blame. The findings were published in Psychiatry Research: Neuroimaging.
Major depressive disorder is a common mental health issue with a relatively high relapse rate. In an effort to reduce the likelihood of relapse, Mindfulness-based Cognitive Therapy (MBCT) trains depressed individuals to respond to negative self-thoughts with acceptance and compassion, and studies suggest that the approach is effective.
Researcher Kate Williams and her colleagues wanted to delve further into the effectiveness of MBCT, by investigating changes in the brain after treatment. As the reduction of self-blame is thought to be a key component in avoiding a relapse into depression, the researchers were particularly interested in examining activation in brain regions associated with self-blame.
A neuroimaging study was conducted among 16 adults who had been in remission from major depression for at least three months. The subjects participated in two-hour sessions of mindfulness-based cognitive therapy on a weekly basis and one all-day session in the sixth week. The subjects took part in a self-blame task both before and after the MBCT, while their functional magnetic resonance imaging (fMRI) activity was recorded.
The self-blame task presented participants with 90 scenarios involving a “negative interaction between themselves and their best friend”. Participants were asked to indicate whether they, their friend, or neither of them were most to blame in each scenario.
First, the MBCT reduced participants’ self-blame when reacting to scenarios where they were depicted acting negatively toward their best friend, or where their best friend was depicted acting negatively toward them. This finding suggests, the researchers say, that the MBCT provided the remitted depressed individuals with ways to “self-protect” when another was acting negatively towards them.
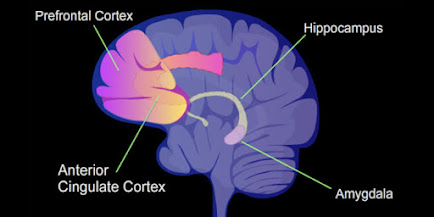
This reduction in self-blame appeared to correlate with neural changes. When researchers contrasted fMRI activity during self-blame versus other-blame, they found a drop in activation of the bilateral dorsal anterior cingulate cortex (dACC) and the medial superior frontal region, following the MBCT. The dACC, the researchers note, has been previously linked to emotions related to self-blame such as guilt and embarrassment.
As Williams and team express, these findings suggest that MBCT “reduces engagement of neural networks associated with salient emotions when feeling self-blame.” Interestingly, the researchers also found that reduced activation in the self-blame versus fixation contrast following MBCT was linked to greater self-kindness as measured by the Self-Compassion Scale. The researchers propose that expanding self-kindness may play a role in the reduction of self-blame through MBCT.
Williams and colleagues emphasize that their study was uncontrolled and relied on a small sample. Future studies, they say, should attempt to replicate these findings in a controlled setting and among a larger sample.
The study, “Changes in the neural correlates of self-blame following mindfulness-based cognitive therapy in remitted depressed participants”, was authored by Kate Williams, Rebecca Elliott, Shane McKie, Roland Zahn, Thorsten Barnhofer, and Ian M. Anderson.



Reacties
Een reactie posten